The decision-making process regarding breast cancer treatment options, specifically breast conserving surgery (BCS) versus mastectomy, is a complex and sensitive matter that takes into account the patient’s preferences and the surgeon’s clinical opinion. A range of anatomical factors, such as tumor size, breast size, and proximity of the tumor to the skin, can influence the surgeon’s recommendation regarding BCS or mastectomy.
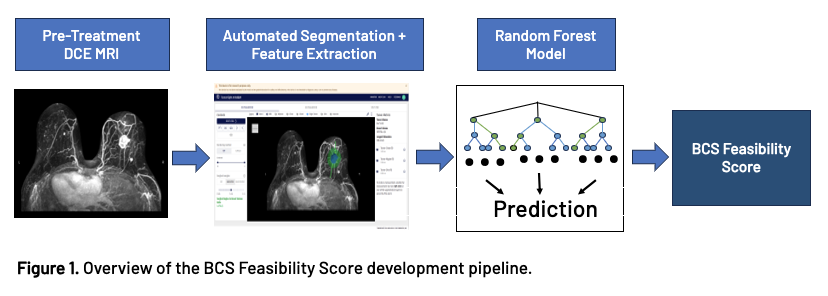
To help facilitate this shared decision-making process we developed the BCS Feasibility Score, a tool capable of predicting the feasibility of BCS based on standard-of-care pre-treatment DCE- MRI.
Methods
The BCS Feasibility Score is generated from a binary classifier machine learning model and represents the probability that a given patient could receive BCS. The score is based solely on the automated segmentation from TumorSight, a software platform that uses only pre-treatment DCE MRI and applies a suite of deep learning algorithms to segment the tumor and surrounding breast tissues. From this multi-tissue segmentation, we extracted 25 spatial morphology features to use in the model development process.
The training and testing sets were a subsample of a publicly available dataset (Duke Breast Cancer MRI; Saha et al, 2018). The total training/testing set consisted of 749 cases, 363 of which received mastectomy and 386 who received BCS. Before model training occurred, we split 20% of the sample to use as the test set. We then trained a random forest classifier across a range of pre-set hyper-parameters, using the 25 spatial morphology features as inputs, and using 5x cross-validation in the training set. After assessing model performance in the test set, a fully independent holdout set with 579 cases [335 (57.9%) BCS, 244 (42.1%) mastectomy] was used as a validation set.
Results
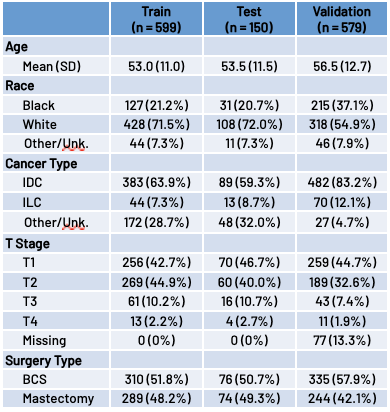
Table 1. Cohort Clinical and Demographic Characteristics
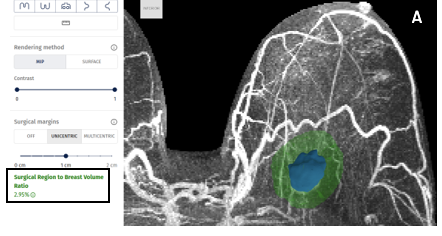
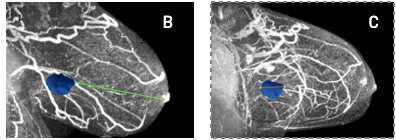
Figure 2. The most predictive features were convex hull volume and tumor to breast volume ratio (A), tumor to nipple distance (B), and tumor longest dimension (C).
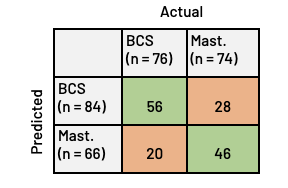
TEST set
We successfully predicted BCS in 56 out of 76 cases (73.7%), and mastectomy in 46 out of 74 cases (62.2%). Overall, we observed an AUC = 0.76 and an F1 score = 0.66, indicating moderate to strong model performance. The most important features in the model, as measured by SHAP values, included the axis aligned tumor longest dimension, tumor to nipple distance, the volume of the tumor convex hull, and the ratio of tumor convex hull volume to breast volume.
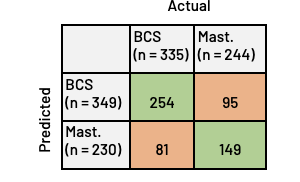
VALIDATION set
We successfully predicted BCS in 254 out of 335 cases (75.8%), and mastectomy in 149 out of 244 cases (61.1%). Overall, we observed an AUC = 0.75 and an F1 score = 0.63. Validation set performance mirrored results observed in the test set, indicating strong generalizability. Comparing patients who underwent BCS to those who underwent mastectomy, we observed significant differences across all four of the most predictive features.
Conclusions
TumorSight and the BCS Feasibility Score can help empower both patients and clinicians with information and tools to facilitate surgical-planning decisions.

