Authors: Vincent J. Reid, MD, FACS1, Linsey P. Gold, DO, FACOS, FACS2, Eric A. Brown, MD, FACS2, Allison A. DiPasquale, MD3, Anne G. Peled, MD4, Joseph R. Peterson, PhD5, Barry S. Rosen, MD5,6
1Mercy, Cedar Rapids, IA, USA; 2Comprehensive Breast Care, Troy, MI, USA; 3Texas Oncology, Dallas, TX, USA, 4Sutter Health, San Francisco, CA, USA, 5SimBioSys, Inc., Chicago, IL, USA; 6Advocate Good Shepherd Hospital, Barrington, IL, USA
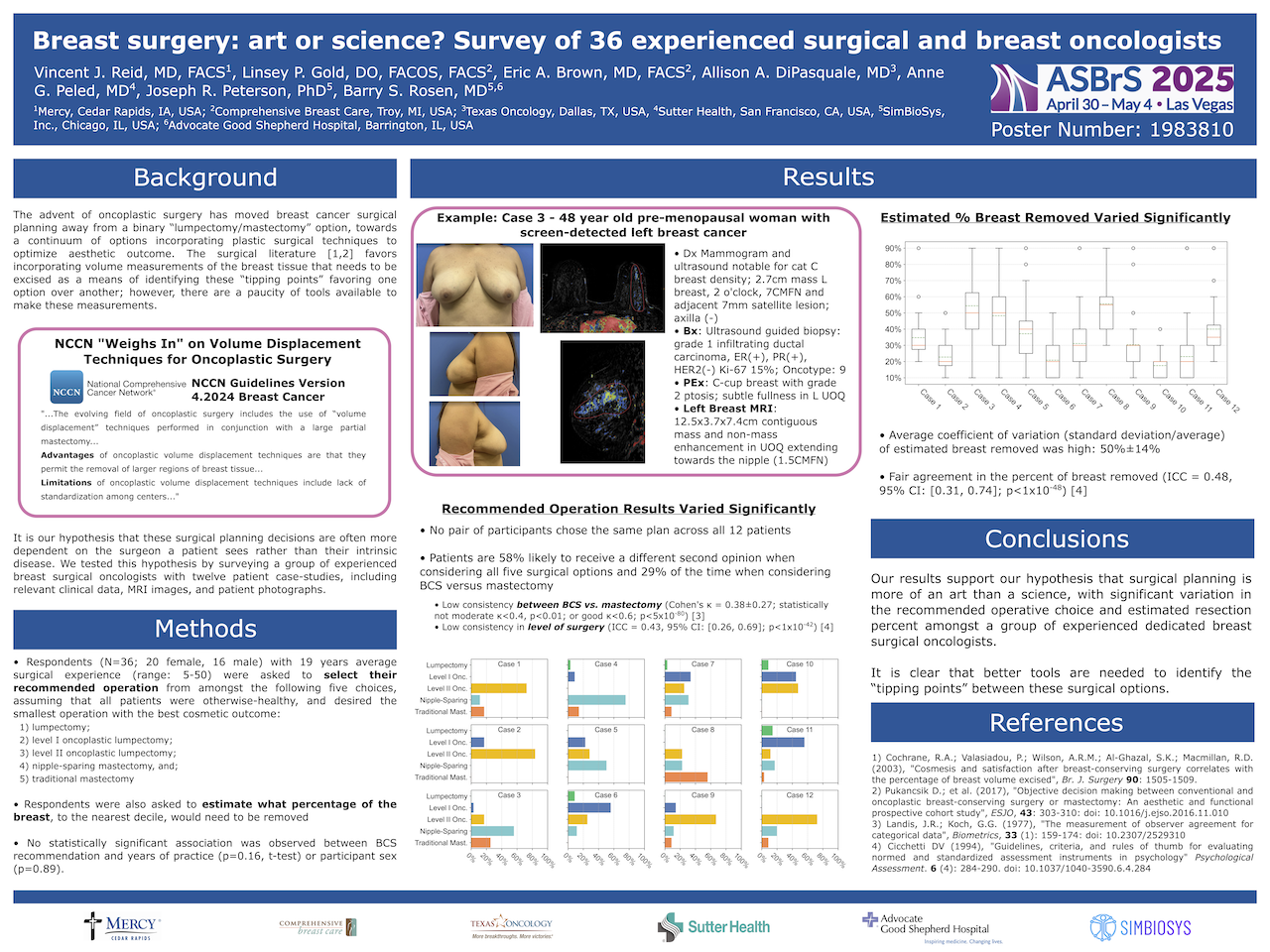
Background: It is our hypothesis that the operation a woman has for breast cancer may be more dependent on the surgeon she sees rather than her intrinsic disease. We tested this hypothesis by surveying a group of experienced breast surgical oncologists with twelve patient case-studies, including relevant clinical data, MRI images, and patient photographs.
Methods: All case-studies included multifocal tumors. Respondents were asked to select their recommended operation from amongst the following five choices, assuming that all patients were otherwise-healthy, and desired the smallest operation with the best cosmetic outcome: lumpectomy; level I oncoplastic lumpectomy; level II oncoplastic lumpectomy; nipple-sparing mastectomy, and; traditional mastectomy. Respondents were also asked to estimate what percentage of the breast, to the nearest decile, would need to be removed.
Results: There were 36 subjects (20 female, 16 male), with an average of 19 years of post-training clinical practice. We calculated each surgeon’s breast conservation (BCS) rate, which varied between 33%–91% (median 66%). No statistically significant association was found between BCS recommendation and years of practice (p=0.16; t-test), or participant sex (p=0.89). We found significant variation in the specific operation chosen; no pair of participants chose the same plan, and only one pair had the same recommendations for BCS versus mastectomy. The likelihood that any two physicians would agree on any surgical plan was 42%±15%; when looking at lumpectomy vs. mastectomy, the likelihood was 71%±16%.
Consistency of BCS versus mastectomy recommendation was assessed by Cohen’s kappa (κ) and found to be fair (κ = 0.38±0.27), but not likely to be moderate (κ<0.4; p<0.01) or good (κ<0.6; p<5×10-80). The consistency of individual surgery type was assessed by intraclass correlation coefficient (ICC). An ICC of 0.43 (95% CI: [0.26, 0.69], p < 1×10-42) was found, corresponding to fair agreement (0.4–0.59) across subjects.
Significant variability was also observed in estimated percentage of breast removed: 28%±12%. Strikingly, the average coefficient of variation (standard deviation over average) for the percentage of breast removed was 0.50±0.14. The ICC for estimated percent of breast removed was 0.48 (95% CI: [0.31, 0.74], p < 1×10-48), corresponding to a fair agreement (0.4–0.59).
Conclusions: It is clear that even amongst an experienced group of breast surgical oncologists, there is significant variation in surgical recommendations. This was evident in the specific type of breast conserving operation, type of mastectomy, and the choice between breast conservation or mastectomy. Indeed, our results indicated that a patient like those included in the study would receive a different second opinion 58% of the time when considering all five surgical options, and 29% of the time when considering BCS versus mastectomy. Breast cancer surgical planning appears to be more of an art than science, and lends itself well to further study to understand the degree of implicit bias in recommendations, and the development of surgical planning tools to reduce variation.

